Neurdegenerative Diseases
Why Early Detection of Alzheimer’s is So Important
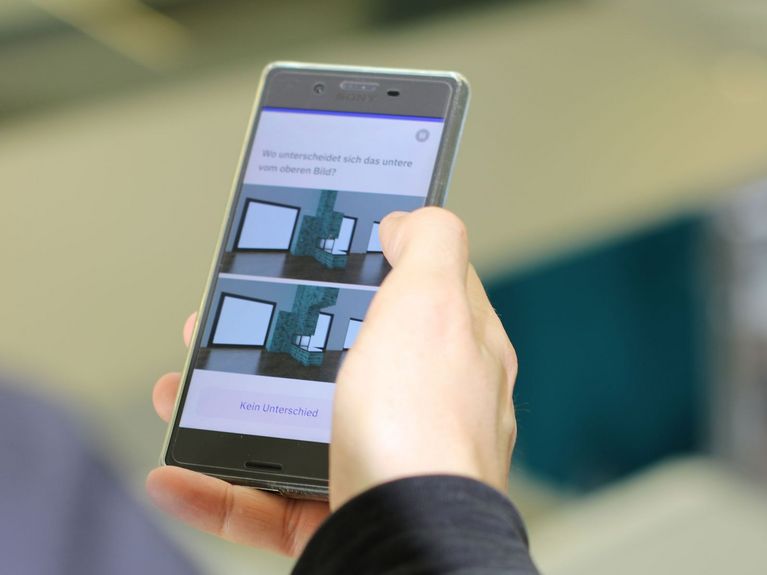
The neotivCare app is designed to provide a meaningful picture of memory performance at an early stage, thus enabling timely intervention. Photo: neotiv
Alzheimer’s dementia is one of the greatest challenges in neurodegeneration. Significant progress in early detection is being advanced at the German Center for Neurodegenerative Diseases (DZNE) in Magdeburg. In addition, new medications offer hope in the fight against the disease.
Emrah Düzel, group leader and clinical coordinator at the DZNE, as well as director of the Institute for Cognitive Neurology and Dementia Research (IKND) at the Otto von Guericke University Magdeburg. Photo: DZNE
Alzheimer’s, the most common form of dementia, is a neurodegenerative disease that often begins decades before the first clinical symptoms appear. Memory problems are a key early symptom, but they also occur frequently in healthy older adults. Early intervention is crucial, as experimental and clinical data show that cognitive and physical training can improve memory functions in older adults, even if they are in the early stages of Alzheimer’s disease.
Emrah Düzel, who leads clinical research focused on Alzheimer’s at the DZNE in Magdeburg and is Director of the Institute for Cognitive Neurology and Dementia Research (IKND) at Otto von Guericke University in Magdeburg, explains: “The disease begins with the accumulation of toxic proteins in the brain. The first signs of this can be detected up to 20 years before the onset of dementia.” Early diagnosis is critical to slowing the progression of the disease.
Alzheimer: Often Diagnosed Too Late
Alzheimer’s is caused by a combination of genetic factors and environmental influences. Age-related changes, cardiovascular diseases, unhealthy lifestyles, and chronic inflammation also contribute to the disease. A key mechanism in Alzheimer’s is the formation of so-called beta-amyloid plaques in the brain, which disrupt communication between neurons and contribute to neurodegeneration. Additionally, tau proteins, also known as neurofibrillary tangles, begin to clump together. Tau proteins usually help stabilize cell structures and organize nutrient transport within cells. However, in Alzheimer’s, these tau proteins change and start to twist into abnormal shapes.
These processes lead to synapse loss and neuronal degeneration, impairing memory and cognition. Alzheimer’s is often diagnosed when a person is in middle to late adulthood, typically from age 65 onward. Diagnosis usually occurs when the disease has progressed, and cognitive symptoms noticeably interfere with daily life. Early detection not only significantly improves the quality of life for patients and their families but also allows for better medical care and targeted treatment.
An App for Early Detection
To address this, the DZNE team, together with Otto von Guericke University and the Magdeburg start-up neotiv, developed an app designed to detect the early signs of the disease and enable timely intervention. The app, called “neotivCare”, includes a series of sensitive cognitive tests that target specific brain regions and highlight subtle cognitive changes. These tests are designed to detect early signs of Alzheimer’s that may not be captured by conventional tests. A key feature of the app is its practicality; patients can take the tests at their convenience in their own environment, reducing the need for frequent doctor visits and extensive testing. The results are provided to the patient’s physician, who can then determine if further examinations are necessary. Düzel explains: “Our tests are designed to be used in a general practitioner’s office without requiring extensive on-site examinations. GPs can prescribe the app, giving patients ample time to complete the tests at home. The results also account for fluctuations over time.”
The app is already being used in clinical trials worldwide. In Germany,“neotivCare” is being implemented in pilot projects with several health insurance companies and has shown promising results in a large study involving over 700 patients. This study, independently evaluated, demonstrates that the app can be an effective complement to traditional diagnostic methods, especially for starting treatment early and making lifestyle changes.
Advances in Treatment
In addition to early detection, new treatment options are critical to improving patients’ quality of life. A major challenge in Alzheimer’s therapy has been the lack of drugs targeting the root causes of the disease, with most medications only addressing its symptoms. Two promising drugs that have recently gained attention in the scientific community are Lecanemab and Donanemab. Lecanemab received full approval in the U.S. in 2023. This intravenous infusion therapy aims to remove beta-amyloid plaques from the brain and has shown in clinical trials to slow the progression of the disease. Over a period of 18 months, the drug slowed cognitive decline by about a quarter. However, in Europe, the European Medicines Agency (EMA) decided against approving Lecanemab in the summer of 2023, leading to disappointment among many professionals and patient organizations. The EMA is currently reviewing its decision.
Donanemab, another drug showing great potential, was also approved in the U.S. in July 2024. Like Lecanemab, it removes beta-amyloid plaques from the brain. In 75 percent of study participants who received the drug in the early stages of the disease, beta-amyloid deposits in the brain were nearly fully cleared after 76 weeks of therapy. Although the drug cannot reverse or completely halt the disease’s progression, there is hope that it can slow cognitive decline. However, both Lecanemab and Donanemab are only effective for individuals in the early stages of Alzheimer’s, when symptoms are not yet significantly affecting daily activities. This makes early detection of Alzheimer’s all the more crucial.
The Path Forward
Advances in early detection and treatment offer new possibilities in managing Alzheimer’s. The app from Magdeburg could see widespread use in clinical practice, helping many individuals detect the disease early. The combination of innovative early detection tools and new therapeutic approaches could fundamentally change the future of Alzheimer's treatment and provide many patients with a better quality of life.
Readers comments